Osteoporosis
•Osteoporosis is a major public health threat for 28 million Americans, 80% of whom are women.
• In the U.S. today, 10 million individuals already have osteoporosis and 18 million more have low bone mass, placing them at increased risk for this disease.
•One out of every two women and one in eight men over 50 will have an osteoporosis-related fracture in their lifetime.
•More than 2 million American men suffer from osteoporosis, and millions more are at risk. Each year, 80,000 men suffer a hip fracture and one-third of these men die within a year.
•Osteoporosis can strike at any age.
•Osteoporosis is responsible for more than 1.5 million fractures annually, including 300,000 hip fractures, and approximately 700,000 vertebral fractures, 250,000 wrist fractures, and more than 300,000 fractures at other sites.
•Estimated national direct expenditures (hospitals and nursing homes) for osteoporosis and related fractures are $14 billion each year.
Bone is living, growing tissue. It is made mostly of collagen, a protein that provides a soft framework, and calcium phosphate, a mineral that adds strength and hardens the framework. This combination of collagen and calcium makes bone strong yet flexible to withstand stress. More than 99% of the body’s calcium is contained in the bones and teeth. The remaining 1% is found in the blood.
Throughout your lifetime, old bone is removed (resorption) and new bone is added to the skeleton (formation). Scientists actually say that every seven years, every bone in your body is new! During childhood and teenage years, new bone is added faster than old bone is removed. As a result, bones become larger, heavier, and denser. Bone formation continues at a pace faster than resorption until peak bone mass (maximum bone density and strength) is reached around age 30.
After age 30, bone resorption slowly begins to exceed bone formation. Bone loss is most rapid in the first few years after menopause but persists into the postmenopausal years. Osteoporosis develops when bone resorption occurs too quickly or if replacement occurs too slowly. Osteoporosis is more likely to develop if you did not reach optimal bone mass during your bone building years.
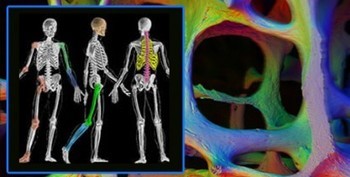
Osteoperosis is essentially a thinning and weakening of the bones that happens to all of us as we age. If this deterioration in the bones goes untreated, our skeleton eventually will become weak and fragile, and some bones will be likely to break or fracture. Women are generally at greater risk of developing Osteoperosis than men.
This is directly due to hormonal changes related to estrogen. Specific areas that seem to be the first to weaken are the spine and hips often leading to pain, disability and functional deficits. There is no method of determining the actual structure of bones without performing special x-ray methods called densitometry. The most advanced modality out today is through Dual Energy X-Ray Absorbtiometery (DEXA).
DEXA is known for its resolution and reproducibility while Densitometry will give accurate and precise measurements of the amount of bone (not their actual quality). This measurement is termed “bone mineral density” or BMD. The World Health Organization (WHO) has established criteria for making the diagnosis of osteoporosis, as well as determining levels which predict higher chances of fractures.
These criteria are based on comparing bone mineral density (BMD) in a particular patient with those of a 25 year old female. BMD values which fall well below the average for the 25 year old female (stated statistically as 2.5 standard deviations below the average) are diagnosed as “osteoporotic”. If a patient has a BMD value less than the normal 25 year old female, but not 2.5 standard deviations below the average, the bone is said to be “osteopenic” (osteopenic means decreased bone mineral density, but not as sever as osteoporosis).
Interestingly, although these criteria are widely used, they were devised in a Caucasian female so there will be some differences when these levels are applied to non Caucasian females or to males in general. Despite this flaw, measurement of BMD is used daily and has proven to be very helpful in all groups. Some men will be subject to increased fracture rates when they have significantly less BMD than the predicted fracture level for women. In other words, some men will be at increased risk for fracture even when they have osteopenia.
Osteoporosis is different from most other diseases or common illnesses in that there is no one single cause. The overall health of a person’s bones is a function of many things ranging from how well the bones were formed as a youth, to the level of exercise the bones have seen over the years.
During the first 20 years of life, the formation of bone is the most important factor, but after that point it is the prevention of bone loss which becomes most important. Anything which leads to decreased formation of bone early in life, or loss of bone structure later in life will lead to osteoporosis and fragile bones which are subject to fracture. Proper treatment can help control the pain and other symptoms while letting you live a more satisfying life.
Exercise is a crucial variable in dealing with Osteoporosis and is a scientifically proven method of treatment. Resistance exercise, under guidance of the proper health professionals will help prescribe a program to stress the bones in a controlled fashion so that the bone mineral content and bone mineral density increases without injury.
Osteoporosis is more common than it should be. Although we don’t know how to completely stop bone loss, we can take steps to prevent many of the fractures. Shown here are the basic building blocks for stronger bones. Prevention starts in childhood, with good nutrition and exercise.
Fall prevention is especially important in elderly persons. Many medical papers focus on medications that can be given to reduce the rate of bone loss. Most lay articles, on the other hand, stress life-style issues such as diet and exercise. BOTH are important!
Sometimes doctors and their patients just want to take a medication for osteoporosis, without paying attention to these basic building blocks of bone health. The medications will not be as effective if there is inadequate calcium and vitamin D in the body. The other building blocks are proper exercise, weight gain and proper over all nutrition, caffeine reduction, smoking cessation and fall prevention in elderly.
Follow some of these general principals to ensure a safe & productive exercise program
1-Exercises that you can perform that are weight bearing in nature are the best (walking, dancing, hiking, stair-climbing). Stressing the bones through its long axis is optimal.
2-Do not perform large impact activities that cause undue jarring to the spine.
3-Resistance exercise can generate tension in the bones thus stimulating the bones to grow. This refers to training with either light weights or elastic bands.
4-Bone density increases the most with higher weights and fewer repetitions.
5-Increase your weight slowly and progress accordingly. Listen to your body.
6-Postural exercises that help you become more upright can reduce stress on specific areas of the body.
7-Balance exercises help maintain equilibrium and reduce the risk of falling. (Explore Tai-chi)
8-Avoid movements to the end of your range (twisting, forward or backward bending).
9-Most studies show that an exercise program of nine months in duration will produce the desired increase in bone mineral density.
10-The frequency of exercise recommended is 3-5 days/week.
11-Always warm-up and cool-down.
12-During activities of daily living, become conscious of your positioning. Bend from the hips to bend down, don’t slouch when you sit and stabilize the lower back with your hand when sneezing or coughing.
13-Remember: Small 10 minute bouts of activity have shown to be just as beneficial as one long bout of exercise.
OSTEOPOROSIS, X-RAY
OSTEOPOROSIS, X-RAY
These are both DEXA scans indicating Osteoperosis of the hip joint.
By determining a patient’s T-score, the physician will see whether a woman has or is at risk for osteoporosis:
T-Score: WHO Criteria for Osteoporosis in Women Normal BMD > -1.0 below the young adult reference range Low Bone Mass (Osteopenia) BMD is -1.0 to -2.5 SD below the young adult reference range Osteoporosis BMD < -2.5 SD below the young adult reference range Severe Osteoporosis BMD < -2.5 SD below the young adult reference range and the patient has one or more fractures.