ACL…ABC’s
An injury to any part of the body can result in pain and loss of function, but an injury to the ACL (Anterior Cruciate Ligament) of the knee can often lead to abnormality of gait, sensations of instability, constant swelling and the inability to participate in sports and recreation. Others have sustained ACL injuries with minimal impairment, but this may be attributed to age, size of the tear, involved structures surrounding musculature and prior history of injury. In fact, 15% of the population can survive happily with a ruptured ACL, so patient profile is imperative for assessing the prognosis.
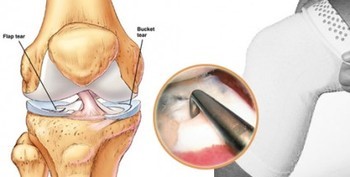
Basically, the ACL is known as the guide wire of the knee. Its main job is to prevent forward translation of the tibia on the femur. That is the forward movement of the lower leg bone (Tibia) on the upper leg bone (Femur). It also helps prevent hyperextension of the knee and is crucial in sports and activities requiring pivoting, changing directions (cutting), jumping and landing. When a ligament is torn, it is called a sprain. Depending on what reference is used, sprains can have different grades relating to the degree of the tear. A first degree tear, being partial disruption of the ligament, while grade 4 is known as a complete tear. Moreover, this is an injury that should not be taken lightly and one should be aware of the related caveats. Subsequently, it is imperative to understand what the proper course of treatment should be and what health care professional can help you along the way to recovery.
An injury to the ACL is usually accompanied by a popping or snapping sound deep in the knee. It can also cause an enormous amount of swelling and muscle guarding just minutes after the injury, making it hard to diagnose by manual skills alone. The patient or athlete may not be able to fully extend their knee and they do not feel comfortable bearing weight on it. An assistive device would be in order to help the patient ambulate safely. At this point, it is advisable to see an orthopedic surgeon for further evaluation. This is due to the fact that it is not uncommon to injure other vital structures in the knee making it a more complicated sequlae. Diagnostic testing using an MRI will usually ensue after the orthopedic visit to further confirm the structures involved. From here, the orthopedic surgeon will decide whether the injury is serious enough for surgical repair or if a course of rehabilitation alone is the way to go. Every doctor has different opinions based on their training and experience, but it usually depends on the age of the patient, health of the knee joint as well as the pursuit of future activity.
There are many different types of surgical techniques to repair the ACL. This topic is beyond the scope of this article, albeit it is of utmost importance to understand the inherent strengths and weakness of the graft chosen in addition to its harvest site. Whatever method of intervention is taken, surgery or not, physical therapy will be extremely important to the outcome of this injury. The main goal of physical therapy is to restore the joint anatomy, provide static and dynamic stability, restore correct ambulation and prepare for return to work or sport. During the first couple of weeks after the injury, the main goal should be to decrease pain and swelling. The second phase should consist of increasing range of motion, gaining hamstring and quadriceps control during weight-bearing activities as well as gaining total lower limb strength. The third phase is involved with increasing proprioception, continuing more complex exercise and the possibility of jogging may enter to the program considering all other milestones are met. Finally, the last and fourth phase is the gradual re-integration to work or sport with the main focus on improving agility, reaction time and a focus on hamstring strength. Many people perseverate on the quadriceps not realizing that the hamstring muscles are the group of muscles that aid the ACL the most. A good final test for the ACL is the single leg hop test. This is simply doing a standing long jump on one leg. The result must be within 3 inches of the non-injured side. If a patient or athlete can perform this comfortably then they are definitely ready to return to work or sport.
Through my experience as both a physical therapist and as a patient who tore their ACL, I find it extremely important to keep three main goals in mind. The first is to regain full extension. Most people focus on flexion so much that they can actually injure the graft before it is revascularized and make it too flexible. The second is to restore your gait as soon as possible. Many people walk asymmetrically for so long that secondary muscles get injured from overcompensating for so long. The last major focal point is to regain the kinesthetic and proprioceptive awareness. It is so common to cease rehabilitation once you can comfortably perform most of your activities of daily living. I can not stress enough the part of therapy that restores the neuro-muscular awareness of the knee. This is where the confidence and mental strength is developed. Ultimately, every stage in the rehabilitative protocol is important for a successful outcome. Make sure you are comfortable and communicate well with your physical therapist. This only ensures success.